Uterine anomalies play an understated role in the common perception of endometriosis.
While they often cause infertility, they can also have an effect on the development of endometriosis. In our own clinical setting, we have found that 38% of our patients who had a mild form of uterine structure abnormality tested positive for endometriosis. This is significant to note as less than 5% of women on average have arcuate uterus upon hysteroscopic evaluation. This means that patients with endometriosis have a statistically higher chance of having an arcuate uterus in comparison to the general population. Therefore, we think it is highly important to shed light on uterine malformations and the impact they can have on endometriosis patients.
Uterine anomalies, also known as uterine malformations, are female genital malformations that often result from abnormal development. They can lead to physical mishappening of the uterus or more subtle abnormalities within the uterine cavity. Some of these differences can cause conditions such as pelvic pain, infertility, and even endometriosis.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Forms of uterine anomalies
Malformations of the uterus can take various different forms, ranging from major uterine cavity physical changes to more subtle abnormalities. A 2011 observational study, assessed 94 patients with abnormal uteri (5.5% of the total population of patients) to determine some of the most common forms of anomalies. The findings included the following:
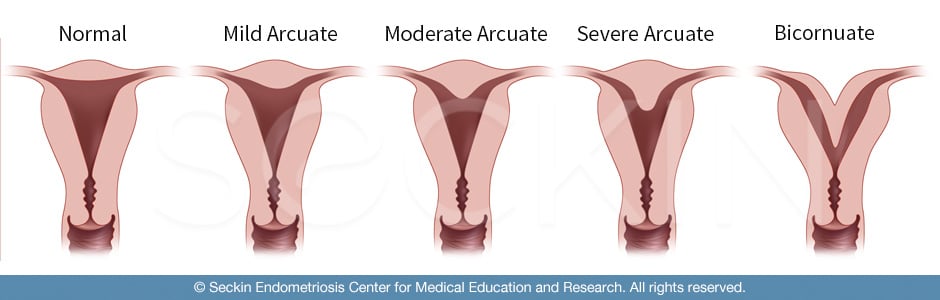
Arcuate uterus
This term has been classically difficult to define but represents a mild form of a septal uterus. The myometrium of the fundus dips inward into the uterine cavity, possibly causing small septation. The myometrium of the fundus is the top portion of the uterus, opposite the cervix. This division is part of the reason why the arcuate uterus is so challenging to define. This is because it can be difficult to discern this from the more pronounced septate uterus. In fact, in Europe, doctors do not even use the term “arcuate uterus”.
However, when defined separately from the septate uterus by having a midline prominence of 1.5 cm or less, the arcuate uterus makes up 70% of uterine abnormalities. This does not have any obstetrical implications, meaning it does not have an association with infertility or miscarriages. However, it has shown some correlations with other gynecological diseases, such as endometriosis. Therefore, it can be highly beneficial to separate the arcuate uterus as a subcategory of a septate uterus.
Septate uterus
This is a malformation in which a septum protruding from the fundus divides the uterine cavity, while the normal outer shape remains intact. Medical theories debate the distinction between arcuate and septate uterus. Recent studies have shown though, that the septate uterus is less common in patients without a history of infertility in comparison to the more subtle form that is the arcuate uterus. In other words, a septate uterus is a common anomaly in women with a history of miscarriages and infertility. There are also rare instances where this septum completely divides the uterine cavity and cervix into two halves (uterine Didelphis or double uterus).
Bicornuate uterus
A bicornuate uterus is a uterine duplication anomaly, which is the result of a partial failure of fusion of the Müllerian ducts (the connection between the uterine cavity and fallopian tubes). It accounts for approximately 25% of congenital uterine anomalies. In a bicornuate uterus, the outer fundal cleft is greater than 1 cm and there is a wide intercornual (tube) distance visible via hysteroscopy and laparoscopy. A simple resection and surgical intervention cannot treat a bicornuate uterus. A bicornuate uterus may increase the risk of recurrent pregnancy loss, cervical incompetence, and possible cerclage placement. A surgeon can use the hysteroscope to explore the two uterine horns and assess the depth and angle of the two horns. Surgical correction can help in cases of reproductive failure but a reproductive specialist should handle this.
Unicornuate uterus
In a unicornuate uterus, or “one-sided uterus”, the uterus is blocked from one side, closing one of the two Müllerian ducts. This abnormality appears as a “banana shape” in imaging tests. It can have a significant effect on fertility including a greater risk of miscarriage, preterm delivery, and in some cases, ectopic pregnancy.
Müllerian agenesis
This uterine anomaly is known as Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. It defines the underdevelopment or complete absence of the uterus. While rare, it has tremendous impacts on the reproductive system as patients are usually infertile and lack a menstrual period.
Effects of uterine anomalies
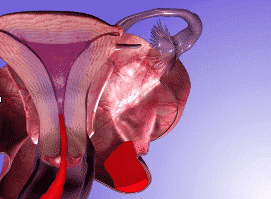
The effects of uterine anomalies can vary from patient to patient. One common complication is that structure anomalies can lead to painful peristalsis (dysperistalsis) and abnormal outflow of menstrual debris. This potentially increases the reflux of retrograde flow, which can participate in endometriosis development. Some normal menstrual flow is expelled out of the uterus. But retrograde reflux blood and debris can also move into the fallopian tubes and pool into the pelvic cavity and peritoneum, leading to endometriosis.
Diagnosis of uterine anomalies
Hysteroscopy or magnetic resonance imaging (MRI) can help diagnose uterine anomalies.
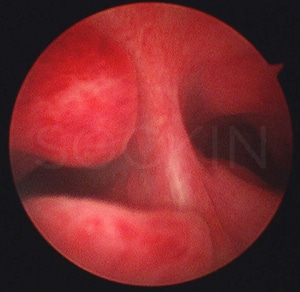
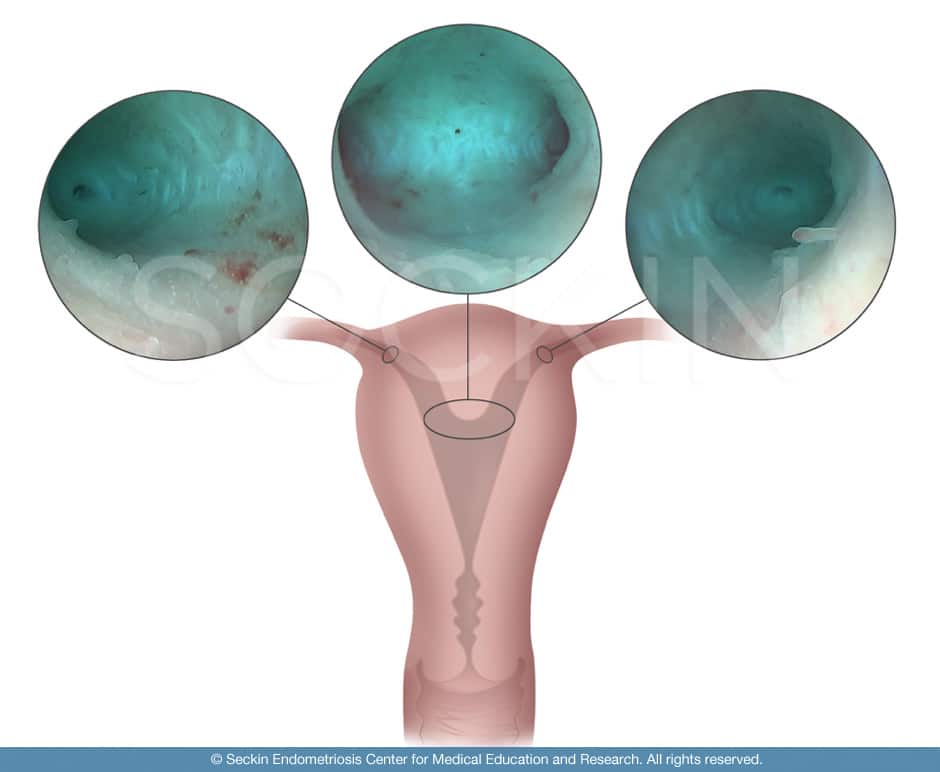
Hysteroscopy
Hysteroscopic evaluation is very important when a patient receives laparoscopic evaluation and surgery. It uses a hysteroscope (camera) to visualize the uterine cavity by inserting the device vaginally. Using this imaging technique, a trained surgeon is able to identify any uterine anomalies. This procedure is a crucial part of any thorough gynecological surgery. It allows the surgeon to assess whether or not a septum appears within the uterine cavity, and if so its extent. Thus any hysteroscopy should be accompanied by laparoscopic surgery for endometriosis.
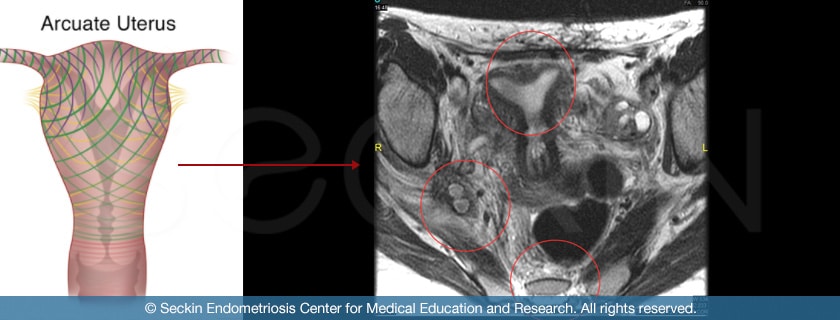
MRI
MRI is a preoperative medical imaging technique used in radiology to form pictures of the inner anatomy and organs. Using magnetic fields and radio waves, an MRI is able to make out abnormal intrauterine structures. This is highly useful in presumptively diagnosing uterine anomalies.
Endometriosis and uterine anomalies
Both obstructive and nonobstructive uterine anomalies are associated with endometriosis. One common explanation for this relationship is the abnormal menstrual flow that occurs with these uterine anomalies.
Reverse peristalsis occurs so sperm can swim upstream and travel into the fallopian tubes and combine with an egg. The coordinated contractions of uterine muscular fibers drive this, which could possibly have differential activation.
In cases of uterine abnormalities, retrograde menstrual debris can take advantage of this pathway and move back into the fallopian tubes, ovaries, peritoneum, and pelvic cavity. All of these areas are common sites for endometrial tissue, stem cells, and inflammatory enzymes contained within this reflux debris to latch onto and eventually develop into endometriosis lesions. Therefore, uterine anomalies can be a cause of endometriosis, secondary to retrograde menstruation.
Endometriosis and arcuate uterus
The arcuate uterus is often considered a normal anatomical variation with questionable reproductive repercussions. However, it must be recognized as a pathological finding in endometriosis patients. In fact, our studies have shown abnormal arcuate architecture and its subtle forms are associated with increased prevalence of both peritoneal and advanced endometriosis. As a result, what an arcuate uterus means for an obstetric patient (infertility case) is different from what it means to an endometriosis patient. Continued testing and identification of arcuate uterus are thus important for endometriosis patients. The potential resection of midline prominence may be a significant step in the treatment of endometriosis.
Our approach
How do we assess uterine anomalies?
At the Seckin Endometriosis Center, we feel that it is crucial to assess the uterine structure and function of each patient. We conduct a hysteroscopy on all of our patients who come in for surgery to assess any uterine abnormalities. We also advise our patients to receive an MRI pre-surgery to provide us with a presumptive understanding of the structure of their uterus.
How do we define an arcuate uterus?
An arcuate uterus is the mildest form of a septal uterus. While it is considered to be a normal variation from an obstetrical standpoint, we have found it to be a much more common anomaly in our endometriosis patients. Therefore, it is highly important to make the distinction between arcuate and septal uteruses. The sub-distinction between the two abnormalities is seen in the differing length of midline protuberance, which we cut off at 1.5 cm. However, we believe that these anomalies should also be defined in a more continuous way, in terms of midline defect or degree of “arcuateness” (ranging from mild to severe).
How do we identify an arcuate uterus?
We always assess these anomalies and this distinction in our surgeries through the use of hysteroscopy.
During this procedure, we aim to surgically identify an arcuate uterus through four key criteria points. These are midline prominence, vertical stria, bilateral cornual funneling, and dilation of tubal Ostia. The first criterion point is seeing whether or not a septum exists by evaluating midline prominence. We then look to identify any vertical stria. These are stretch marks that can exist when the uterus is misshapen, such as when the fundus concaves inward. The next key component to evaluate is the Müllerian ducts. These are common sites for abnormalities to take place in arcuate uteruses due to abnormal development during development.
Our data on uterine anomalies
Our clinical research data has shown that endometriosis patients are prone to having uterine abnormalities, specifically arcuate uterus.
Of the 260 hysteroscopies we performed from 2015 to 2016, 100 (38%) showed arcuate uterus and minor variations. The remaining 160 (62%) had a normal uterus. This is a notable similarity to what previous research has shown i.e. 37% of endometriosis patients have an arcuate uterus.
While this is not a majority, it is significant because arcuate uterus occurs in less than 5% of all women according to recent studies. In nearly 60% of our 100 patients, excision specimens came back positive for endometriosis. The remaining specimens showed inflammation and fibrosis. Moreover, 39 cases (39%) with an arcuate uterus were positive for endometrioma. Conversely, only 38 out of 160 normal (24%) uterine cases were positive for endometrioma. This means that uterine anomalies brought a 1.76-fold increase in the incidence of ovarian endometrioma. These endometriomas, in turn, can lead to further development of endometriosis to the point of stage 3 or 4 deep infiltrating endometriosis.
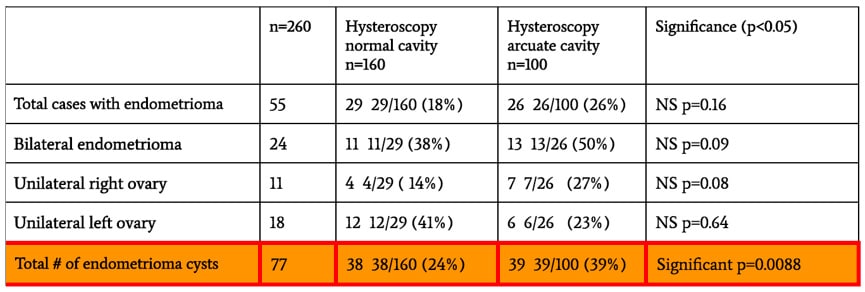
Therefore, identification of arcuate uterus through hysteroscopy is important for endometriosis patients. It also suggests that potential resection of midline prominence may be a significant step for the surgical treatment of endometriosis patients.
What we do
At the Seckin Endometriosis Center, we take great care in understanding our patients, both from a surgical and personal perspective. Endometriosis patients are some of the strongest women around, and they deserve the strongest care. We take great pride in assuring that no stone goes unturned in each case. Assessing uterine abnormalities and their possible effects is no exception.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.