Endometriosis is one of the most underdiagnosed, misdiagnosed, and mistreated diseases in women of reproductive age. Because the first step to receiving successful treatment is a proper diagnosis, it is imperative to find an endometriosis surgeon who will use and review all diagnostic tools at his or her disposal. This includes imaging techniques such as sonography, MRI, and laparoscopy. Another crucial tool for diagnosing that often goes underappreciated is a physical exam. This entails the patient providing a thorough overview of their symptoms and past medical history.
It is important to find a surgeon who will listen to these symptoms, which may include painful periods, painful sex (dyspareunia), gastrointestinal distress such as constipation especially in young women, painful bowel movements, and diarrhea. These symptoms can be highly suggestive indicators for a presumptive endometriosis diagnosis. It is key to find a surgeon who is not only knowledgeable but also compassionate and patient enough to listen to your full story, as these elements can help make up a highly accurate, but still speculative, diagnosis.
What are the steps to diagnosing endometriosis?
Diagnosing endometriosis requires three levels of diagnostic evaluation:
Step 1: diagnosing endometriosis pre-surgery
The initial stage is a clinical examination and appropriate testing, which includes a pelvic examination and ultrasound. During this time, patients thoroughly recount their current symptoms. The doctor intently listens in order to build the trust necessary to facilitate long-time care. Upon physical examination, findings such as the cervix, pelvic side, and posterior thigh tenderness, which can radiate as far back to the cervix at the rectal wall, serve as key signs of the presence of endometriosis lesions and their possible locations. Sonogram technology can help confirm the cause of this tenderness. If you have diffuse pelvic tenderness, a rectal exam may also be necessary as it is important to determine if there is localized rectovaginal tenderness, a key sign of rectovaginal disease.
Step 2: diagnosing endometriosis during surgery
The second stage is a visual diagnosis by recognition of endometriotic lesions through laparoscopy. This will take place in the operating room, during laparoscopic surgery.
Step 3: diagnosing endometriosis after surgery
The final formal diagnosis of endometriosis requires the pathologic examination of lesions under a microscope. Surgical specimens obtained through laparoscopic deep excision surgery must be sent off to the lab. It usually takes a few days following your surgery to assess those specimens.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
What testing takes place pre-surgery?
Pelvic exam
This physical examination of a patient’s pelvis and pelvic organs is part of any fully comprehensive gynecological exam. During this exam, a physician will look for any and all points of pelvic tenderness. Through a pelvic exam, your doctor will be able to gain a better understanding of your symptoms and any pain you may be experiencing. If your physician specializes in endometriosis, they may even be able to diagnose conditions like frozen pelvis.
Transvaginal ultrasound
An ultrasound is a safe and painless technique that uses sound waves to produce detailed images of the inside of the body. The doctor inserts a small probe, called a transducer into your vagina in a way similar to the way you would insert a tampon. Sound waves will then pass harmlessly from the transducer through the skin. They then bounce off certain organs and tissue in the body and create “echoes.” These echoes reflect back to the transducer, which converts them into electrical signals in order to produce an image. The images are viewed in real-time on a monitor and are also recorded and photographed for your physician to review. It is important to note that this test can be performed during menstruation.
Sonohysterography
During this imaging technique, the doctor injects fluid through the cervix into the uterus. They then use ultrasound to produce images of the uterine cavity. The use of this fluid provides more detail of the inside of the uterus than ultrasound alone. This procedure is performed to find the underlying causes of abnormal uterine bleeding, miscarriage, and infertility. It can help detect abnormal uterine growths like fibroids or polyps, uterine scarring, and abnormal uterine shape.
This procedure cannot be scheduled during your menstrual cycle or when you are experiencing abnormal bleeding. In cases of abnormal bleeding, the test can take place as soon as the bleeding stops. After this exam, you may have some cramping, spotting, and watery discharge. The procedure is generally safe, but in rare cases, there is a risk of pelvic infection.
Magnetic resonance imaging (MRI)
MRI is a non-invasive imaging technique that produces a strong magnetic field and radio waves. These are used to create detailed images of the tissues, organs, and other areas.
An MRI differs from a CT scan as it uses low-frequency magnetic fields as opposed to the high-energy X-rays that a CT scan uses, which often puts patients at risk of radiation exposure. An MRI produces much more comprehensive and detailed imaging than an ultrasound, as it often encompasses the entire body. However, an MRI is much more expensive than an ultrasound. Moreover, MRI testing does not take place in the office of your everyday primary care physician or gynecologist but you need a referral.
Nevertheless, MRI testing serves as a very useful tool for your doctor to have an idea of the extent of your disease. So, it is very common for your specialist to ask for an MRI test prior to surgical treatment.
What testing takes place during surgery?
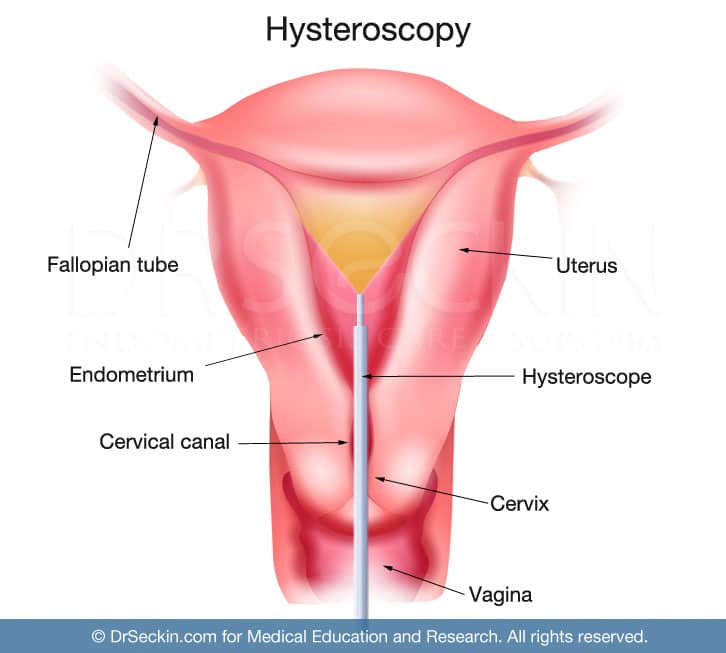
Hysteroscopy
Hysteroscopy is an imaging technique performed in the operating room in order to view the lining of the uterus (endometrium). This is done using a thin tool with a light and camera (the hysteroscope) attached to its tip. The doctor gently inserts this into the vagina, through the cervix, and into the uterus. With this technique, a surgeon will be able to see if there is any uterine cause for heavy menstrual bleeding, pelvic pain, or infertility. This is very useful in cases of adenomyosis.
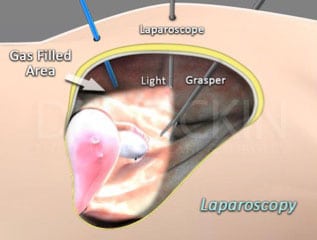
Laparoscopy
Laparoscopy allows the visualization of the abdomen and pelvic cavity through an instrument known as the laparoscope. Performed under general anesthesia, the laparoscope is inserted through small incisions made in the abdominal and pelvic cavity. The surgeon then sutures these back together after surgery. The goal of this technique is to make small incisions in order to ensure minimal invasion. This method allows your surgeon to inspect the abdominal and pelvic regions (and beyond, as needed) to diagnose and subsequently remove endometrial lesions, utilizing his or her surgical modality and tool of choice like a laser or excision clippers.
Why is diagnosing endometriosis difficult?
Endometriosis exists in different forms with different symptoms, signs, and prognoses. Increased awareness of the disease has given rise to an increase in diagnoses. However, endometriosis still remains a seldom recognized and poorly understood illness. Confusion about appropriate management continues to surround it.
How is endometriosis formally diagnosed?

Despite advances in diagnostic technologies and other presurgical imaging tests that help determine, a confirmation of endometriosis requires a surgical biopsy. This is commonly obtained through minimally invasive laparoscopy.
Are there other ways to formally diagnose endometriosis?
Ultrasounds, MRI, CT scans, and endometrial biopsy samples can be part of a diagnostic workup. But to date, anything less than surgical confirmation of endometriosis is considered uncertain. There are also no specific blood tests to diagnose endometriosis.
Our approach to diagnosing endometriosis pre-surgery
Physical exam
There are a variety of tests that we perform to diagnose endometriosis before a patient has surgery.
After we note your symptoms, history, and complaints during a consultation, we will conduct a thorough physical exam. This consists of a comprehensive pelvic exam, which includes inspecting the cervix, checking for neuropathy in your lower back and legs, assessing costovertebral angle (CVA) tenderness, and evaluating the upper vagina with digital palpation. We evaluate the nodularity, thickening, and shortening of the uterosacral ligament, rectovaginal, cul-de-sac, and lateral vaginal walls in this manner. The tenderness of these areas is significant in measuring the extent of the disease.
We will also perform a gentle, single digital pelvic bimanual examination. In addition, we also note the mobilization and tenderness of the cervix to touch during this exam (CMT, or cervical motion tenderness). We will then evaluate the anterior and posterior cervix and the upper vagina with digital palpation.
Transvaginal ultrasound
For patients experiencing painful bowel movements, we perform a transvaginal rectovaginal sonogram (transvaginal ultrasonography or transvaginal ultrasound) on top of a physical exam. Transvaginal ultrasound performed after a bowel preparation improves the ability to properly diagnose intestinal lesions. It also provides invaluable details including which layers of the intestine the disease affects and the distance between the lesion(s) and the anal border. We carefully evaluate the uterine walls, endometrial canal, and endometrial cavity for the presence of adenomyosis, fibroids, and polyps. We then scan the cul-de-sac and rectovaginal septum. Finally, it is important to inspect the ovaries. Having treated women with endometriosis for nearly three decades, we strongly believe that ovarian cancer is directly associated with endometriosis. Transvaginal ultrasounds have consistently proven to be the most promising imaging method for the routine screening of ovarian cancer. It is also very effective in screening for endometriosis.
Sonohysterography
We use sonohysterography along with an ultrasound to produce detailed images of the uterine cavity in order to aid in identifying endometrial lesions of submucosal fibroids and polyps particularly in patients with a history of infertility and heavy periods, regardless of their pain.
Our approach to diagnosing endometriosis during surgery
Hysteroscopy
Before any excision surgery, we conduct a hysteroscopy in order to visualize the lining of the uterus (endometrium). This will allows us to see if there is any uterine cause for heavy menstrual bleeding, pelvic pain, or infertility.
Laparoscopy
Following your hysteroscopy, we make small incisions into the abdominal and pelvic region. We then insert a laparoscope into the incision sites. The images appear on two monitors, one for the surgeon and one for the attending resident. We do all our surgeries via laparoscopy. This allows us to clearly visualize any suspected endometriosis lesions.
ABC technique (™)
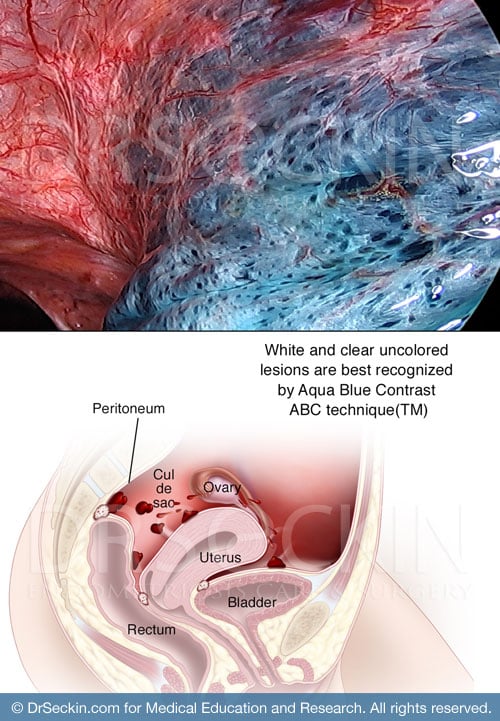
The Aqua Blue Contrast Technique (ABC) is a patented surgical technique that we use during laparoscopic excision surgery in order to clearly visualize endometriosis scar tissue with an aqua blue contrast solution. While some lesions may be invisible to the typical surgeon using laparoscopic light, the ABC technique eliminates light reflection and allows the surgeon to visualize, and thus identify and fully excise endometriosis lesions. This method ensures that we identify all areas of endometriosis development throughout the body. This diagnostic tool is strictly unique to us.
So many patients diagnosed with endometriosis undergo multiple surgeries, only for their symptoms to return. Often, this occurs because the surgeon has not identified every endometriosis lesion and left behind a considerable amount of scar tissue. In order to ensure a thorough and successful surgery, it is crucial for you to ask the right questions about your surgery, and to learn how your surgeon will identify and excise endometrial lesions.
Using common diagnostic tools such as ultrasound, MRI, and hysteroscopy, in combination with our unique method of laparoscopy using the ABC technique, we ensure that no visible endometriosis lesion goes undetected. But on top of these diagnostic tools, the first step in identifying your endometriosis is through proper communication.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.
