There is no cure for Endometriosis. However, several surgical and non-surgical methods exist to manage the disease, alleviate symptoms, and avoid infertility. Of these, laparoscopic deep excision surgery is the “gold standard”.
The surgeons at the Seckin Endometriosis Center (SEC) have many years of experience in dealing with the most complex of deep infiltrating endometriosis (DIE) lesions and have been able to provide long-lasting relief to their patients.
Dr. Tamer Seckin is among the handful of specialists to have trained under Dr. Harry Reich, who pioneered laparoscopic hysterectomy back in 1989.
Endometriosis laparoscopic surgery
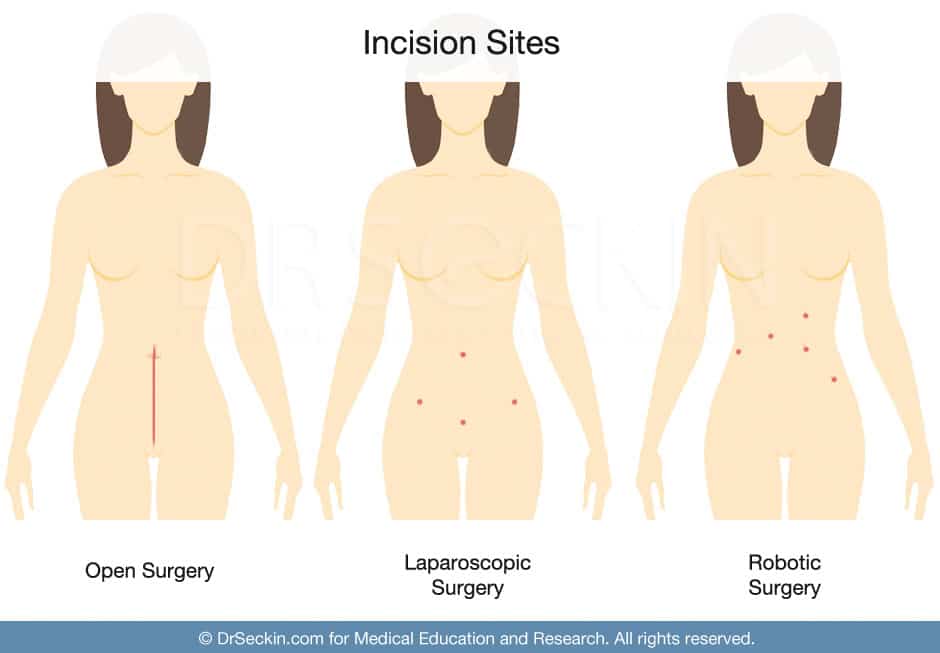
Laparoscopy, also known as keyhole excision surgery, is a type of minimally invasive surgery. Unlike open endometriosis treatment surgery, minimally invasive endometriosis laparoscopic surgery is done via small incisions that allow the entry of tiny cameras and tubes. This allows for more precision, fewer post-operative complications, reduced scarring, and shorter recovery times.
In laparoscopy, each incision is called a port. Your surgeon inserts instruments such as the laparoscope camera, surgical tools, and a tube to pump gas into the abdomen through these ports. The gas helps inflate the abdomen for better accessibility.
The surgeon then lets out the gas and sutures the incisions. It is possible to go back home the same day after the procedure. However, your doctor will often advise for an overnight stay.
Laparoscopy can help in both the diagnosis and treatment of endometriosis.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Limitations of current techniques
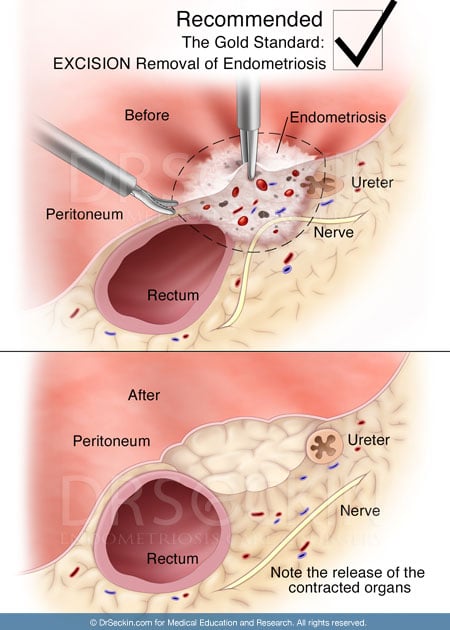
Before trying to understand why laparoscopic deep excision surgery is the most effective in thoroughly removing all endometriosis lesions, we will look into some of the limitations of current approaches:
- Laser ablation removes only the top layer of the lesion and does not remove it from within. Also, laser ablation can potentially scar surrounding healthy tissue as well.
- The use of heat or high energy for excision also leaves behind burnt tissue that can cause additional pain.
- Many surgeons do not have the adequate training to properly differentiate various types of endometriosis lesions. This is mainly because of the inability to properly visualize the lesions in the backdrop of the light source.
- Reconstruction and proper suturing of the incision are essential to aid repair and ensure a full recovery.
- Lack of understanding about pan-systemic spread of endometriosis (such as thoracic or bladder endometriosis) and dearth of multidisciplinary approaches to tackle it.
- Use of robotic-assisted laparoscopic techniques that do not match up to the precision and tactility of manual interventions.
Our approach to laparoscopic excision surgery
With years of experience, Dr. Seckin’s team at SEC has developed ways of overcoming the above challenges and improving surgical outcomes while retaining the patient’s natural fertility to the maximum possible extent.
Manual excision
We follow a more hands-on approach in order to properly differentiate between scars, adhesions, and lesions while navigating inside the body. This is simply not possible with robotic-assisted laparoscopic techniques since the surgeon has no tactile feeling of the tissue and must rely solely on video information. Also, the incisions made by robotic assistance are larger compared to those made manually by experienced surgeons.
Dr. Harry Reich, the pioneer of laparoscopic hysterectomy, strongly favors a manual approach. This way, the surgeon can feel the disease and get a proper assessment of the severity.
The lone clinical trial (LAROSE) that compared conventional and laparoscopic methods also found that there is no real benefit in terms of perioperative conditions or quality of life between the two.
Enhanced visualization strategy
We use a patented Seckin’s Aqua Blue Contrast (ABC) technique that changes the color of the peritoneum by hydro-floatation with a contrast color and retroperitoneal distention.
The advantage of the ABC technique is that it enables the surgeon to clearly visualize all available lesions even in the background of the operating light. Therefore, it becomes easy to effectively identify and isolate all visible lesions and scarring for maximum recovery.
Complete excision surgery
An endometriosis lesion is like an iceberg with just the peak being visible while the actual bulk of the lesion is still within the underlying tissue. The underlying part of the lesion can regrow again leading to recurrence of symptoms. Therefore, complete excision of all visible endometriosis lesions is essential for full symptom alleviation and to prevent a recurrence.
During deep excision surgery, we “core out” the lesion completely from within, so that there is no residual lesion present. This results in almost no recurrence rates in the long term and faster recovery times.
Cold excision surgery
We believe a “cold excision surgery” approach is best to preserve healthy tissue function. We do not use electricity or high energy to remove scars. This alleviates the risk of burnt tissue and further complications. This also helps us in working with pathology teams to confirm the presence of endometrial tissue in the scar, thus providing a confirmed diagnosis of endometriosis.
Multidisciplinary approach
Endometriosis can affect not only the peritoneum and organs in the pelvic region but can also spread to other parts of the body. Treating extra-pelvic endometriosis requires involving specialists from multiple disciplines to ensure positive treatment outcomes.
At Seckin Endometriosis Center, we always follow a multidisciplinary approach that draws from the expertise of several specialties. These include pathologists, anesthesiologists, gastroenterologists, urologists, thoracic surgeons, psychologists, radiologists, and more.
Having a multidisciplinary team helps us to collectively review and provide accurate, symptom-specific advice to our patients along with positive post-operative coping strategies to ensure a smooth recovery.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.