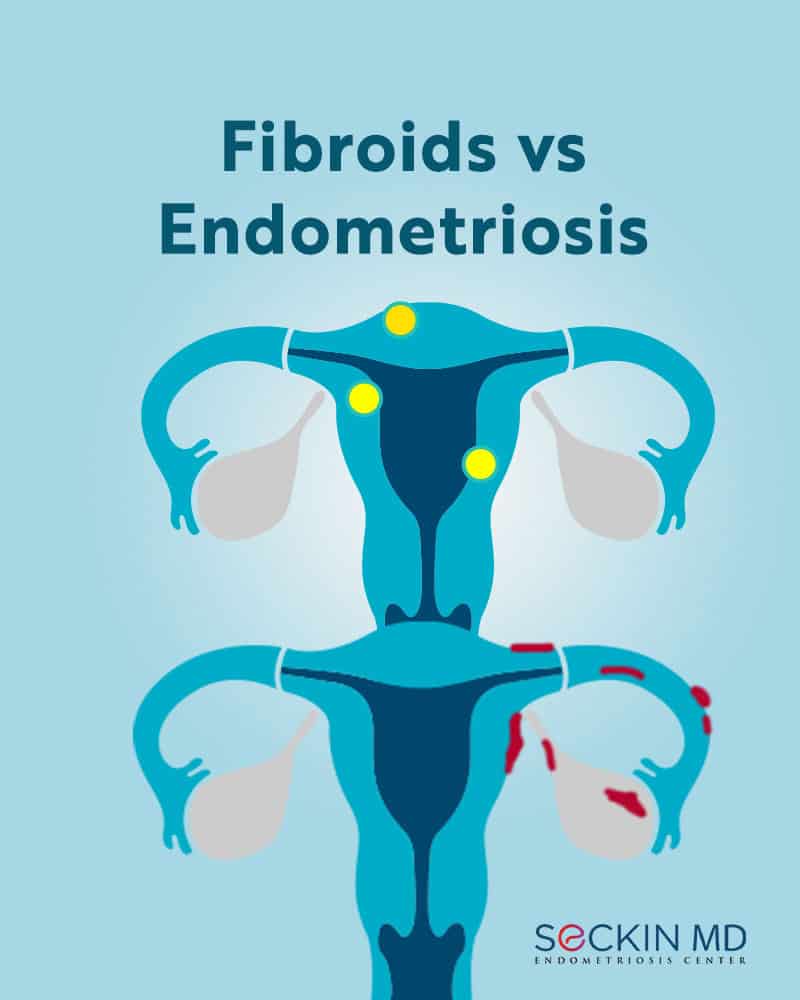
Fibroids vs Endometriosis
Uterine fibroids and endometriosis are diseases that both occur in women of reproductive age, and can both greatly affect their quality of life. Fibroids and endometriosis are also the leading causes of hysterectomy (removal of the uterus).
Here are some of the prominent features of both diseases:
Nature
Fibroids, also known as uterine leiomyomas, are benign growths originating from the uterus that can manifest in a variety of numbers and sizes. Fibroids primarily consist of smooth muscle and fibrous tissue in the uterus. Doctors classify them based on their localization as intramural, subserosal, submucosal, intracavitary, and cervical. The location and relative size of the fibroid is greatly correlated with the symptoms suffered. For example, a fibroid on the inner lining of the uterus (submucosal or intracavitary) will more likely cause heavy bleeding than a fibroid growing on the outer edge of the uterus (subserosal or pedunculated), which may cause more pain and discomfort when large in size.
Endometriosis, on the other hand, is the growth of endometrial-like tissue outside the uterus within the pelvic and abdominal cavity. This extraneous endometrial tissue also responds to female hormones just as the normal endometrium inside the uterus would. But this tissue has no way to leave the body. This leads to inflammation and scarring at the site of endometrial growth. Endometriosis is classified into four stages based on severity. However, these stages do not always correlate with the severity of symptoms.
Causes
The exact cause of neither fibroids nor endometriosis is clear.
Researchers think that genetic factors, hormonal changes, and the influence of growth factors may all play a role in fibroid formation.
In the case of endometriosis, causative factors may include retrograde menstruation, the transformation of peritoneal cells into endometrial tissue, and the transformation of embryonic cells into endometrial-like cells. Genetic factors may also play a role in increasing risk of developing endometriosis.
Risk factors
Risk factors impacting fibroid development include age (between 30 and 50), ethnicity (Afro-Caribbean descent), high BMI, vitamin D deficiency, high alcohol consumption, and low consumption of green vegetables.
In the case of endometriosis, risk factors include being of reproductive age (between 25 and 40), never having beared children, a family history of the disease, high fat and alcohol consumption, high estrogen levels, and a history of menstrual complications (heavy bleeding, pain with periods).
However, women can have fibroids or endometriosis without the involvement of the above risk factors.
Prevalence
The prevalence of fibroids in various populations can range between 4.5% and 68.6%. However, these numbers are not always consistent since they include both symptomatic and asymptomatic cases. Black women are the most affected. Around 80% of black women develop fibroids by age 50 and have higher incidents of recurrence.
Endometriosis affects around 10% of women of reproductive age worldwide. However, the prevalence is higher (30 to 50%) in women with infertility. This ratio can go up to 70% in women with chronic pelvic pain.
Though both fibroids and endometriosis are independent diseases, symptomatic endometriosis and symptomatic uterine fibroids can co-exist in many cases. However, advanced stages of these diseases usually do not appear together.
Symptoms
Fibroids are largely asymptomatic and only about 20 to 50% of affected women experience symptoms. Uterine fibroid symptoms typically include prolonged, heavy menstrual bleeding (menorrhagia) that can include clots, pelvic pain, frequent yet difficult urination, anemia, fatigue, constipation, and painful intercourse (dyspareunia).
In endometriosis, about 20 to 25% of the cases are asymptomatic, though most symptoms manifest around the time of menstruation. Painful menstrual period (dysmenorrhea) and chronic pelvic pain are among the most common symptoms. Dyspareunia (pain with sex), infertility, painful bowel movements, feeling of abdominal bloat, neuropathy, cramps, back pain, fatigue, constipation, and blood in the urine are some of the other symptoms of endometriosis.
Pathophysiology
Endometriosis is an estrogen-dependent disease while fibroids are progesterone-dependent.
Fibroids look like round nodules of smooth muscle tissue. They can sometimes be attached to the uterus via a stalk (pedunculated fibroids) giving them a mushroom-like appearance. Unlike adenomyosis, which is much more diffuse, fibroids are usually singular with well-defined borders.
The pathophysiology of fibroid formation is still unclear. Apart from the risk factors indicated above, there may be several other factors leading to fibroid formation. These include increased progesterone and estrogen levels, increased expression of transforming growth factor-beta in the extracellular matrix, epigenetic changes, and increased cytokine production. Fibroids also have higher estrogen and estrogen receptor levels along with increased progesterone.
Endometriotic lesions are typically described as being superficial “powder-burn” in appearance. The lesions may start out clear in color and progress from red to black and finally, to white as they mature and fibrosis (scarring) takes place.
While retrograde menstruation is the most widely accepted theory in what causes ectopic (out of place) endometrial tissue, another hypothesis, called coelomic metaplasia is also a theory to be considered regarding the origin of endometriosis. This coelomic metaplasia theory is the transformation of the coelomic epithelium (a type of intra-abdominal tissue) into endometrial tissue. Endometriosis tissue also contains estrogen and progesterone receptors similar to the endometrium within the uterus. Endometriosis is an estrogen-dependent disorder. So, higher levels of estrogen lead to disease progression while increased progesterone levels can result in disease regression.
Diagnosis
Both fibroids and endometriosis are often underdiagnosed and/or misdiagnosed.
Doctors may suspect fibroids during a routine pelvic examination. Confirmatory diagnosis tests include imaging techniques such as ultrasound, saline hysterosonography, and magnetic resonance imaging (MRI). Surgical techniques include hysteroscopy and laparoscopy. Fibroids near the fallopian tubes can be visualized using a special X-ray contrast technique called hysterosalpingography (HSG).
Doctors may also suspect endometriosis during a pelvic exam. Imaging techniques such as ultrasound, hysterosonography, and MRI can help visualize endometrial lesions. Surgical techniques such as laparoscopy provide a better view of the abdominal cavity. At Seckin Endometriosis Center, we use a patented Aqua Blue Contrast (ABC) technique that helps clearly visualize endometriosis scar tissue. This makes it possible to excise every single lesion. The biopsy of surgical specimens obtained via laparoscopic deep excision surgery provides the final and definitive confirmation of endometriosis.
Treatment
Since most fibroids are normally asymptomatic, non-cancerous, rarely interfere with fertility, and shrink after menopause, many doctors advise a wait and watch approach.
Non-surgical treatments for fibroids include GnRH agonists, progestin-releasing IUDs, tranexamic acid, and non-steroidal anti-inflammatory drugs (NSAIDs). These medications do not necessarily shrink fibroids but can help in symptom management. However, larger fibroids usually require surgical interventions such as myomectomy and hysterectomy.
Hysteroscopic myomectomy allows the removal of smaller, intra-uterine fibroids vaginally. Myomectomy can also be performed by laparotomy (open abdominal surgery) or laparoscopic (minimally invasive keyhole surgery), particularly with intramural and subserous fibroids that are located deeper in the uterine wall. Minimally invasive surgery requires skill and meticulous suturing of the uterus to make it viable for pregnancy after the procedure.
Like fibroids, endometriosis symptoms can also be managed using medications or hormone therapy. However, laparoscopic excision surgery is the gold standard and the most advanced treatment option for endometriosis. The highly-trained surgeons at Seckin Endometriosis Center can permanently remove all forms of endometriosis and adhesions with minimal risk of damage to healthy tissue to provide the greatest pain relief.
Hysterectomy (complete removal of the uterus) is advocated in both diseases only as a last resort when all other options fail and the patient is certain that she does not want to further bear any children.
Did you receive a diagnosis of fibroids or endometriosis? Please share your experience with Seckin Endometriosis Center and comment on our post on Facebook or Instagram.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.