Interstitial Cystitis and Endometriosis: The Evil Twins
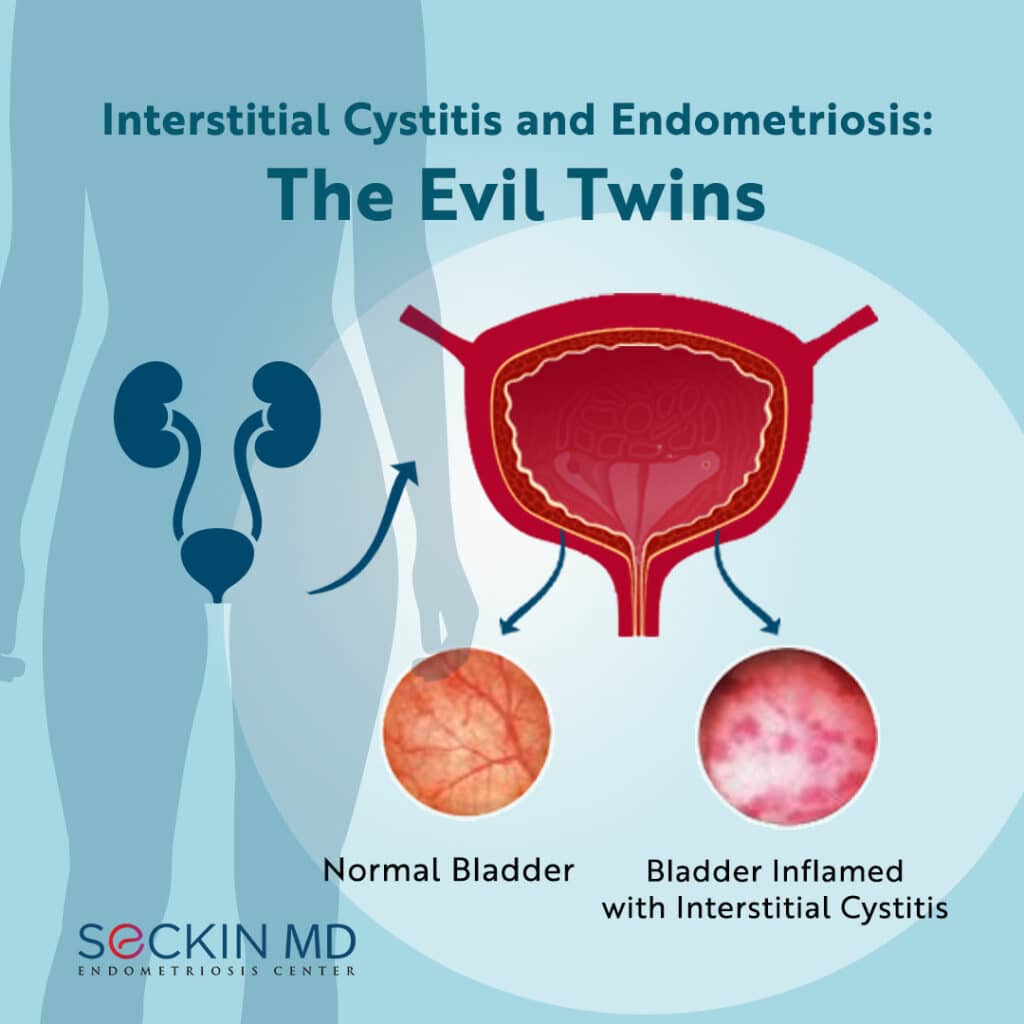
Interstitial cystitis (IC), also known as painful bladder syndrome, is a chronic condition characterized by a feeling of pain and pressure in the bladder. The bladder pain can also manifest as pelvic pain and ranges in severity from mild to severe. The condition mostly affects women and can negatively impact overall quality of life.
Why are endometriosis and interstitial cystitis considered “evil twins”?
Endometriosis and interstitial cystitis share many similar symptoms and are common contributors to chronic pelvic pain. Although endometriosis is one of the major causes of chronic pelvic pain, recent evidence suggests that interstitial cystitis can also play a significant role.
Particularly, the symptoms of interstitial cystitis often overlap with that of bladder endometriosis. These include chronic pelvic pain, an urgency to urinate, blood in the urine, frequent urination throughout the day and night, pain or discomfort during bladder filling, pain during urination, and pain during sex. Endometriosis may be more likely to be in the picture if these symptoms also coincide with menstruation.
While bladder symptoms should not be taken lightly, it is not possible to confirm interstitial cystitis without first excluding endometriosis.
What causes interstitial cystitis?
No one knows the exact cause of interstitial cystitis, but the condition tends to occur in people with a defective epithelial (surface) lining in the bladder that causes caustic or acidic substances in the urine to irritate the bladder wall.
Some of the other causes of interstitial cystitis include:
- release of histamine and other chemicals from a type of immune cell called mast cells
- substances in the urine that can damage the bladder
- changes in nerve cells that register pain in the bladder
- autoimmune attack on the bladder
How does it affect the overall quality of life?
interstitial cystitis results in many complications that can adversely impact a person’s overall quality of life. These include:
- reduced bladder capacity
- frequent urination and pain in the bladder that affects social, personal, and professional life
- emotional stress with the possibility of leading to depression
How do doctors diagnose interstitial cystitis?
Interstitial cystitis can be difficult to diagnose and distinguish from endometriosis.
Laparoscopic deep excision surgery followed by a histological examination is the only gold standard in diagnosing endometriosis. If endometriosis lesions are not present during excision surgery, or if symptoms recur within the first 12 months of surgery, interstitial cystitis should be considered as a possible cause.
A diagnosis of interstitial cystitis can include taking a medical history or a voiding diary, performing a pelvic exam, and a urine test. Your doctor may also ask you to fill out a questionnaire called the Pelvic Pain and Urgency/Frequency (PUF) scale to screen for urinary behavior, pelvic pain, and pain during intercourse.
Your doctor may prescribe a urodynamic evaluation to measure bladder pressure as it fills and empties. Those with interstitial cystitis have smaller bladder capacities and likely pain during filling.
Doctors can also diagnose interstitial cystitis using cystoscopy or by a potassium sensitivity test (PST). In cystoscopy, the doctor inserts a camera into the bladder, which is full of fluid. He or she then drains the fluid to look out for small bleeding areas on the bladder surface. A biopsy is performed by collecting samples from these surfaces to confirm interstitial cystitis.
In PST, the doctor places water in the bladder via a small catheter. He or she then drains the water and replaces it with a potassium chloride solution. Healthy people do not respond to this change, but those with interstitial cystitis feel pain and discomfort. If the patient feels pain, the doctor uses a rescue solution to numb the bladder. The potassium sensitivity test is not very common anymore due to the discomfort it can cause patients. PUF scores often correlate with a positive PST.
Is there a treatment?
Lifestyle and dietary changes to prevent symptom flare-ups can help manage interstitial cystitis. Limiting stress, and eliminating foods one by one such as citrus, tomatoes, coffee, alcohol, carbonated drinks, and chocolate, is one way to see whether bladder symptoms improve.
Prescription drugs approved by the U.S. Food and Drug Administration (FDA) for interstitial cystitis include oral pentosan polysulfate and topically administered dimethyl sulfoxide (DMSO) through bladder instillation. The exact mechanisms by which these drugs work is not fully clear. They most likely restore the protective coating of the bladder. It may be necessary to take the medication for three to six months before symptoms start improving. However, it is usually effective in only about 30 percent of patients.
Other treatment options include antihistamines such as hydroxyzine, antidepressants such as amitriptyline, heparin, and neuromodulation therapy such as transcutaneous electrical nerve stimulation (TENS) and sacral nerve stimulation, Botox injections, and immunosuppressants such as cyclosporine.
If endometriosis is present, laparoscopic deep excision surgery is the gold standard to remove superficial and deep endometriosis lesions in the bladder for lasting symptom relief. The doctor may also perform bladder ulcer cauterization if there are ulcers in the bladder. This may offer temporary symptom relief for up to a year and may need to be repeated if symptoms recur.
Did you receive a diagnosis of Interstitial cystitis? Do you also have endometriosis? Please share your story by leaving a comment on our post on Facebook or Instagram.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.